Virtual Library | Uveitis Causes and Treatment
Uveitis is an ocular condition that occurs when the uveal tract within the eye becomes inflamed, which can lead to alterations in vision, intraocular pressure and comfort. Read on for common clinical signs, how we test for the condition, causes, and treatment options.
← Flip through our digital brochure
Uveitis is inflammation of the uveal tract, the vascular tissue within the eye. This tissue plays many roles in the overall health of the eye. It provides nutrients to ocular structures, helps regulate intraocular pressure, supports the important barrier between the blood and the eye, maintains clarity of the fluid within the eye and supplies nutrition to the retina (an important structure for vision). Disorders of the uvea often lead to alterations in vision, intraocular pressure and comfort.
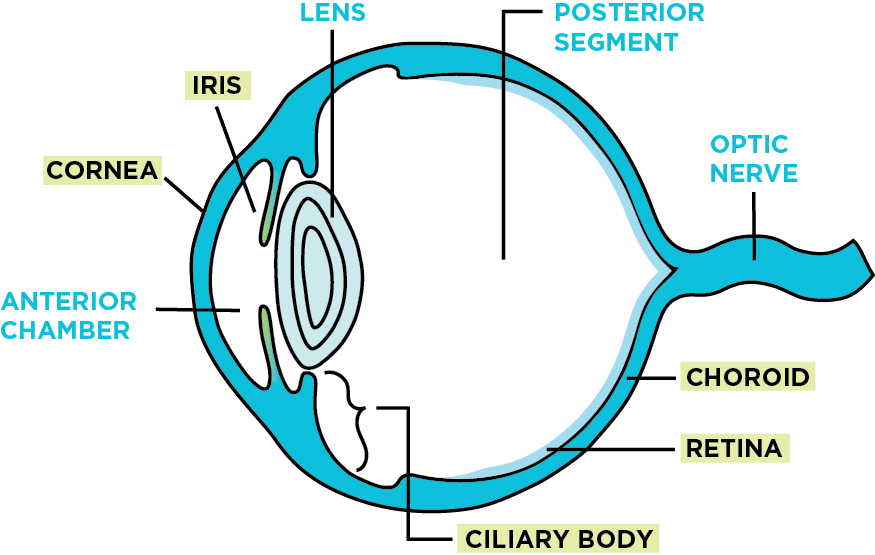 The uveal tract is composed of three parts:
The uveal tract is composed of three parts:
- Iris, or colored part of the eye
- Ciliary body, located just behind the iris, which forms the fluid within the eye
- Choroid, located in the back of the eye behind the retina
The specific pathophysiology of uveitis depends on the underlying cause, but in all cases, there is a breakdown of the blood-eye barrier that normally keeps cells and large proteins from entering the eye. When the uveal tract becomes inflamed, white blood cells can enter the eye and cause damage to the eye. Based on the primary location of entry, uveitis is subclassified into anterior uveitis (inflammation of the front of the eye), posterior uveitis (inflammation of the back of the eye) or panuveitis (inflammation of all portions of the eye).
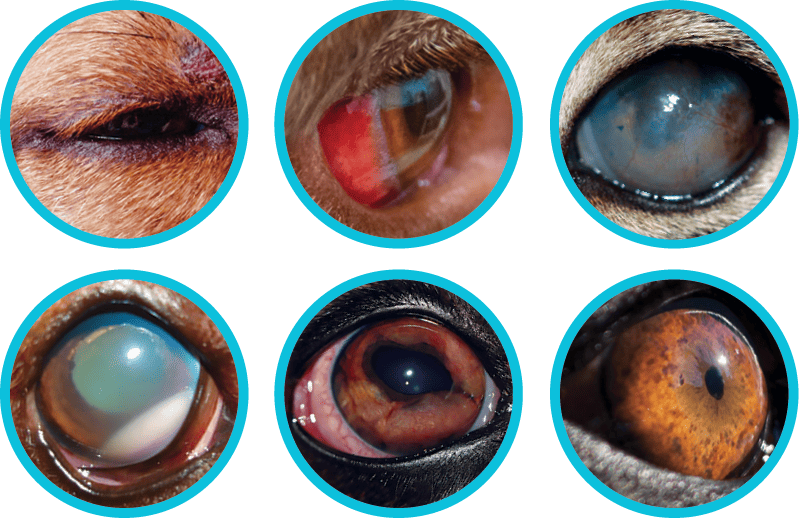
Common clinical signs of uveitis include: squinting, tearing, red eye, cloudy cornea, hazy anterior chamber, blood or white blood cells in the bottom of the eye, change in iris color or shape, swollen iris, small pupil and decreased vision.
It can be difficult to determine the cause of uveitis. Determining one, however, is necessary due to the potential threat to vision or the possibility of a more significant systemic disease.
The top three causes of uveitis fall into the broad categories of infectious, immune-mediated, and neoplastic disease, however, uveitis can also occur secondary to disease of the lens, or other metabolic, vascular, traumatic, toxic, or reflexive causes.
Common causes of uveitis in dogs and cats include auto-immune issues, trauma, high blood pressure, cataract formation, or secondary to systemic infection or cancer. It also may occur secondary to a corneal ulcer, known as reflex uveitis.
Finally, in approximately 50% of cases in dogs and cats, we are unable to find a specific underlying cause, and consider the uveitis to be idiopathic. This diagnosis is made by exclusion, meaning we have to rule out the other more serious causes first before reaching this diagnosis.
Anti-inflammatory corticosteroids and non-steroidal medications are the primary therapy for uveitis. These include both topical eye drops and oral medications. Oral antibiotics may be started if an infection is suspected, or prophylactically. Other treatments considered include mydriatic/cycloplegic therapy (pupil dilator to help relax the muscle that causes the pupil to constrict), oral pain medications, and specific therapy based on the underlying cause.
We often recommend pet patients return for a pressure check within the first few days after diagnosis to make sure that glaucoma (high pressure within the eye) has not developed. If the patient is doing well at home, we suggest they return for a recheck every 1-2 weeks until the disease is in remission. Once the inflammation is controlled, we gradually reduce the medical therapy and continue to closely monitor the pet for any signs of a relapse.
It is important to monitor these cases closes closely, because in some cases, there may be complications to uveitis that may lead to glaucoma, permanent vision loss, retinal detachment or cataract formation.
If monitored and treated appropriately, most cases of uveitis will be controllable, and pet patients will maintain their comfort and vision on a long-term basis.
DID YOU KNOW?
Golden Retrievers can get a special type of heritable uveitis called pigmentary uveitis, or Golden Retriever uveitis. We keep an eye out for this when examining breeding dogs.


We often recommend pet patients return for a pressure check within the first few days after diagnosis to make sure that glaucoma (high pressure within the eye) has not developed. If the patient is doing well at home, we suggest they return for a recheck every 1-2 weeks until the disease is in remission. Once the inflammation is controlled, we gradually reduce the medical therapy and continue to closely monitor the pet for any signs of a relapse.
It is important to monitor these cases closes closely, because in some cases, there may be complications to uveitis that may lead to glaucoma, permanent vision loss, retinal detachment or cataract formation.
If monitored and treated appropriately, most cases of uveitis will be controllable, and pet patients will maintain their comfort and vision on a long-term basis.
Uvetis DDX:
- Infectious
- Bacterial
- Septicemia / endotoxemia
- Leptospira sp.
- Borrelia burgdorferi
- Brucella sp.
- Bartonella spp.
- Fungal
- Blastomyces sp.
- Histoplasma capsulatum
- Cryptococcus spp.
- Coccidioides immitis
- Aspergillus sp.
- Rickettsial
- Ehrlichia canis, Ehrlichia platys
- Rickettsia rickettsii
- Protozoal
- Toxoplasma gondii
- Leishmania donovani
- Parasitic
- Dirofilaria immitis
- Toxocara spp.
- Baylisascaris spp. (ocular larval migrans)
- Taenia multiceps
- Angiostrongylus vasorum
- Viral
- Canine adenovirus types 1 and 2 (immune-mediated)
- Canine distemper virus
- Canine herpesvirus 1
- Rabies virus
- Algal
- Prototheca spp
- Geotrichia spp.
- Bacterial
- Immune-mediated
- Immune-mediated vasculitis
- Immune-mediated thrombocytopenia
- Uveodermatologic syndrome (Vogt-Koyanagi-Harada-like syndrome)
- Inherited
- Pigmentary uveitis in the Golden Retriever
- Idiopathic
- Neoplastic / Paraneoplastic
- Lymphosarcoma
- Ciliary body adenocarcinoma
- Intraocular melanoma
- Hemangiosarcoma
- Other primary and metastatic neoplasms
- Granulomatous meningoencephalitis
- Lens-associated
- Cataract-induced (phacolytic; immune-mediated)
- Lens capsule rupture (phacoclastic; immune-mediated)
- Lens luxation
- Metabolic
- Diabetes mellitus (lens-induced)
- Hyperlipidemia
- Vascular
- Systemic hypertension
- Hyperviscosity syndrome
- Polycythemia
- Coagulopathy
- Periarteritis nodosa
- Trauma
- Blunt trauma
- Penetrating trauma
- Corneal foreign body
- Toxic
- Prostaglandin derivatives (latanoprost)
- Sulfamethazine-trimethoprim (immune-mediated)
- Reflex uveitis
- Keratitis
- Episcleritis
- Scleritis
So, You Brought Home a Bulldog
Cataracts and Cataract Surgery
Cherry Eye / Prolapsed Nictitans Gland and Replacement
Corneal Endothelial Degeneration
Entropion Causes and Treatment
Feline Herpesvirus and Treatment
OFA Certification Registry Exams
Visit our blog, In Focus, to learn more about the pets we see, the treatments we offer and the services we provide to help your pet “see a better life.”